What Is Aortic Stenosis (AS)?
Your heart has four valves that work to keep blood flowing in the right direction.
Think of your aortic valve as “the exit door" of your heart. It's where your heart meets your body's largest artery — the aorta.
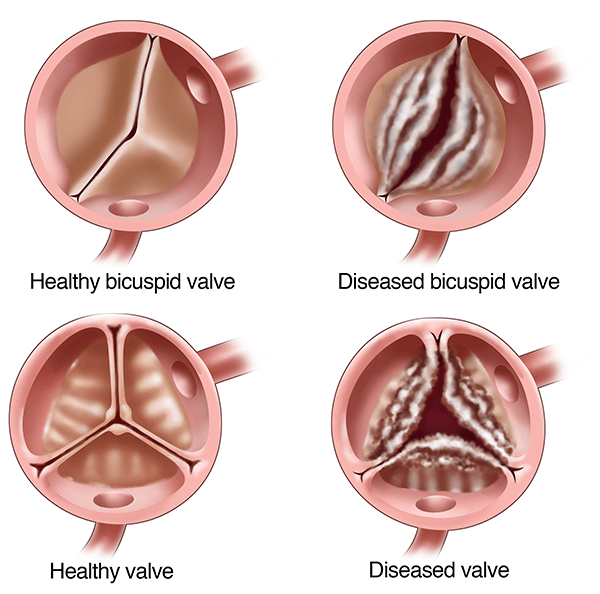
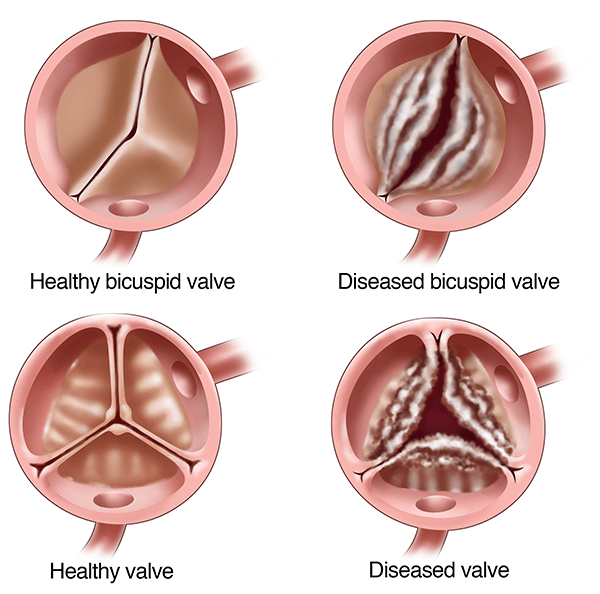
Your aortic valve has three parts, called flaps or leaflets, which connect to the annulus ring.
In a healthy heart, when the left chamber squeezes, blood flows out of it. The flaps of the aortic valve open to let blood flow through.
When the heart relaxes, the flaps snap shut to prevent blood from flowing backward.
The term stenosis is the narrowing of an internal part of the body.
In AS, the valve doesn't open wide enough and limits blood flow from the heart into the aorta. In response, your heart works harder to pump enough blood to meet your body's needs.
Over time, this can cause your heart to weaken and can lead to heart failure.
At UPMC, we take a team-based approach to tailoring the right aortic valve stenosis treatment to your unique needs.
Aortic stenosis causes
AS is common heart disease. It affects about 5% of people over the age of 70.
Although it's sometimes present at birth, AS is more common in older adults.
As you age, calcium deposits in your aortic valve can cause it to stiffen and not correctly open. This narrowing may lead to heart failure and a range of other issues.
1-2% of people are born with a bicuspid aortic valve — a heart defect that can lead to AS.
Doctors often don't notice it in babies and growing children, and it may not cause problems until adulthood. Over time, the aortic valve may get tight or leaky.
Aortic stenosis risk factors
Factors that increase your risk of AS include:
- Age. It often occurs in people older than 65 years.
- Atherosclerosis. A disease of buildup in the artery walls causing them to harden. This condition can go hand in hand with aortic stenosis.
- Bicuspid aortic valve. A condition in which the aortic valve has two flaps instead of three. This can cause the valve to leak or narrow.
- Diabetes mellitus. People with diabetes are more likely to get aortic stenosis because it may speed up plaque buildup in the arteries.
- High cholesterol. Having high cholesterol can cause inflammation and lead to aortic stenosis.
- Rheumatic fever. An infection that can cause the scarring of the heart's valves.
- End-stage kidney disease. Aortic stenosis tends to progress more quickly in people with chronic kidney disease.
Aortic valve stenosis complications
AS can lead to problems, such as:
- Heart failure. Aortic stenosis makes the heart muscle work harder, which weakens it over time, leading to failure. Look for symptoms, including fatigue, shortness of breath, and swelling of the legs, ankles, and feet.
- Endocarditis. This is a bacterial infection within your heart. People with aortic stenosis have a harder time fighting it.
Aortic stenosis prevention
AS is a progressive condition.
Ways to help prevent it include:
- Forming heart-healthy habits.
- Controlling cholesterol and blood pressure.
- Managing diabetes may help prevent stenosis.
See your UPMC heart doctor regularly. Ongoing follow-up care is vital to check your heart disease for possible progression.
Aortic stenosis is a condition in which your aortic valve does not open widely enough to allow adequate blood flow from your heart to your aorta.
Learn more from the UPMC HealthBeat blog: