What Is Diabetic Retinopathy?
Diabetic retinopathy is an eye disease that results from a loss of blood flow and oxygen to the retina.
The retina is in the back of the eye. It collects light and turns it into a signal the brain translates as vision.
Diabetic retinopathy can cause problems ranging from minor blood and plasma leaks in the retina to total blindness. In fact, it's a leading cause of blindness in U.S. adults and often affects both eyes.
There are two kinds of diabetic retinopathy:
- Non-proliferative. This type can cause mild bleeding, swelling, and fatty deposits in the retina.
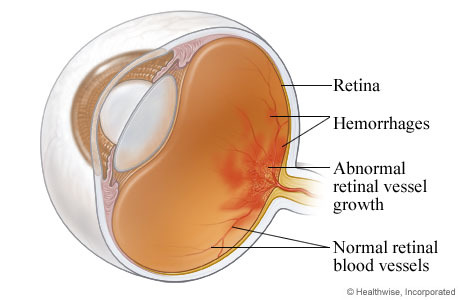
- Proliferative. This kind occurs when blood sugar is out of control. High sugar levels cause widespread blood vessel damage. The retina grows new, abnormal vessels to survive. This can lead to bleeding in the eye, retinal detachment, and even complete vision loss.
Diabetic Retinopathy
Diabetic retinopathy is a disease of the retina, the thin tissue that lines the back of the eye. The condition is a complication of diabetes. It is related to long-term high blood sugar levels. Over time, this leads to changes in blood vessels that interfere with oxygen delivery to the cells in the retina.
Back to top.
What Are the Main Causes of Diabetic Retinopathy?
Diabetic retinopathy occurs when the retina doesn't get enough blood.
People who have had diabetes for longer that isn't well controlled are at greater risk. It's vital to control your diabetes to lower your risk of diabetic retinopathy.
Diabetic retinopathy can happen to anyone with diabetes. This includes type 1, type 2, and gestational (diabetes during pregnancy).
Diabetes while pregnant can speed up the pace of retinopathy, so eye exams during the first trimester are crucial.
The longer your diabetes goes unmanaged, the more likely you will have eye problems.
What are the risk factors and complications of diabetic retinopathy?
Risk factors
Diabetic retinopathy affects about 40% of all people with type 1 diabetes and 20% of those with type 2.
Other risks include:
- The first trimester of pregnancy, if the mother has diabetes or gets gestational diabetes.
- High blood pressure in people with diabetes.
- High cholesterol in people with diabetes.
- Diabetic kidney disease.
Keeping your blood sugar at the right level can reduce the chance of diabetic retinopathy.
Diabetic retinopathy complications
Untreated diabetic retinopathy may lead to:
- Diabetic macular edema. This disease happens when the blood vessels in the retina leak fluid into the macula. The macula is part of the retina you need for central vision.
- Complete vision loss due to problems from proliferative diabetic retinopathy.
Back to top.
Diabetic Retinopathy Symptoms and Diagnosis
What are the warning signs and symptoms of diabetic retinopathy?
You may not notice any symptoms in the early stages of the disease. This is why routine eye exams are so important.
When you do notice symptoms, they may include:
- Vision changes that may come and go (from blurry to clear and back again).
- Trouble reading.
- Problems seeing faraway objects.
- An increasing number of floaters.
- A dark spot in the middle of your vision.
- Dark spots or streaks that look like cobwebs.
- Poor night vision.
- Decreasing vision.
How do you diagnose diabetic retinopathy?
The earlier that your doctor diagnoses your diabetic retinopathy, the better.
That's why it's crucial to have yearly dilated eye exams. Screening exams with photos of your retina also can be very helpful.
During a dilated eye exam, the doctor:
- Places drops in your eyes that open the pupil.
- Thoroughly checks the back of the eye.
- Can see any signs of diabetic retinopathy before you have symptoms.
Anyone with diabetes should have an eye exam at least once a year.
To diagnose diabetic retinopathy, your eye doctor will:
- Give you a complete eye exam, including dilating your eyes.
- Discuss your health history.
- Ask about the medicines you're taking, so bring a full list.
- Look at any recent test results, which you should bring.
Back to top.
What Are the Treatment Options for Diabetic Retinopathy?
Once your doctor has diagnosed the disease and how severe it is, they'll create a tailored treatment plan.
Diabetic retinopathy treatment may include:
- Laser procedures.
- Medicine that can treat both leakage and bleeding in the retina (called anti-angiogenic drugs).
- Surgery to remove the clear gel (vitreous) that fills the middle part of your eye.
Can doctors fix diabetic retinopathy?
If caught early through an eye exam, diabetic retinopathy may be reversible.
At the very least, early treatment can stop it from getting worse.
Can diabetic retinopathy heal itself?
No. It will not get better on its own.
Making lifestyle changes in the early stages may reverse it, but later stages require treatment.
You need to see an eye doctor for routine exams. They can check for signs of the disease and find the best course of treatment.
What's the best treatment for diabetic retinopathy?
Your eye doctor can suggest the best treatment for you. It may depend on how advanced your eye disease is and your health.
No matter what diabetic retinopathy treatment your doctor suggests, it's vital to manage your diabetes. Keeping your blood sugar under control will help keep your eyes healthy.
Back to top.
Contact Us For Diabetic Retinopathy Care
To plan a visit to the UPMC Vision Institute, call 412-647-2200 or 800-446-3797.
By UPMC Editorial Staff. Last reviewed on 2023-10-17.