
3/4/2024
PITTSBURGH — A new smartphone app developed by physician-scientists at UPMC and the University of Pittsburgh, which uses artificial intelligence (AI) to accurately diagnose ear infections, or acute otitis media (AOM), could help decrease unnecessary antibiotic use in young children, according to new research published today in JAMA Pediatrics.
AOM is one of the most common childhood infections for which antibiotics are prescribed but can be difficult to discern from other ear conditions without intensive training. The new AI tool, which makes a diagnosis by assessing a short video of the eardrum captured by an otoscope connected to a smartphone camera, offers a simple and effective solution that could be more accurate than trained clinicians.
 “Acute otitis media is often incorrectly diagnosed,” said senior author Alejandro Hoberman, M.D., professor of pediatrics and director of the Division of General Academic Pediatrics at Pitt’s School of Medicine and president of UPMC Children’s Community Pediatrics. “Underdiagnosis results in inadequate care and overdiagnosis results in unnecessary antibiotic treatment, which can compromise the effectiveness of currently available antibiotics. Our tool helps get the correct diagnosis and guide the right treatment.”
“Acute otitis media is often incorrectly diagnosed,” said senior author Alejandro Hoberman, M.D., professor of pediatrics and director of the Division of General Academic Pediatrics at Pitt’s School of Medicine and president of UPMC Children’s Community Pediatrics. “Underdiagnosis results in inadequate care and overdiagnosis results in unnecessary antibiotic treatment, which can compromise the effectiveness of currently available antibiotics. Our tool helps get the correct diagnosis and guide the right treatment.”
According to Hoberman, about 70% of children have an ear infection before their first birthday. Although this condition is common, accurate diagnosis of AOM requires a trained eye to detect subtle visual findings gained from a brief view of the eardrum on a wriggly baby. AOM is often confused with otitis media with effusion, or fluid behind the ear, a condition that generally does not involve bacteria and does not benefit from antimicrobial treatment.
To develop a practical tool to improve accuracy in the diagnosis of AOM, Hoberman and his team started by building and annotating a training library of 1,151 videos of the tympanic membrane from 635 children who visited outpatient UPMC pediatric offices between 2018 and 2023. Two trained experts with extensive experience in AOM research reviewed the videos and made a diagnosis of AOM or not AOM.
“The eardrum, or tympanic membrane, is a thin, flat piece of tissue that stretches across the ear canal,” said Hoberman. “In AOM, the eardrum bulges like a bagel, leaving a central area of depression that resembles a bagel hole. In contrast, in children with otitis media with effusion, no bulging of the tympanic membrane is present.”
The researchers used 921 videos from the training library to teach two different AI models to detect AOM by looking at features of the tympanic membrane, including shape, position, color and translucency. Then they used the remaining 230 videos to test how the models performed. 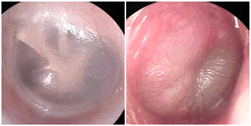
Both models were highly accurate, producing sensitivity and specificity values of greater than 93%, meaning that they had low rates of false negatives and false positives. According to Hoberman, previous studies of clinicians have reported diagnostic accuracy of AOM ranging from 30% to 84%, depending on type of health care provider, level of training and age of the children being examined.
“These findings suggest that our tool is more accurate than many clinicians,” said Hoberman. “It could be a gamechanger in primary health care settings to support clinicians in stringently diagnosing AOM and guiding treatment decisions.”
“Another benefit of our tool is that the videos we capture can be stored in a patient’s medical record and shared with other providers,” said Hoberman. “We can also show parents and trainees — medical students and residents — what we see and explain why we are or are not making a diagnosis of ear infection. It is important as a teaching tool and for reassuring parents that their child is receiving appropriate treatment.”
Hoberman hopes that their technology could soon be implemented widely across health care provider offices to enhance accurate diagnosis of AOM and support treatment decisions.
Other authors on the study were Nader Shaikh, M.D., Shannon Conway, Timothy Shope, M.D., Mary Ann Haralam, C.R.N.P., Catherine Campese, C.R.N.P., and Matthew Lee, all of UPMC and the University of Pittsburgh; Jelena Kovačević, Ph.D., of New York University; Filipe Condessa, Ph.D., of Bosch Center for Artificial Intelligence; and Tomas Larsson, M.Sc, and Zafer Cavdar, both of Dcipher Analytics.
This research was supported by the Department of Pediatrics at the University of Pittsburgh School of Medicine.
PHOTO DETAILS: (click images for high-res versions)
First photo:
CREDIT: UPMC
CAPTION: Alejandro Hoberman, M.D., professor of pediatrics and director of the Division of General Academic Pediatrics at the University of Pittsburgh School of Medicine and president of UPMC Children’s Community Pediatrics.
Second photo:
CREDIT: Alejandro Hoberman
CAPTION: Images of eardrums from a healthy patient (left) or with acute otitis media (right) captured by the new smartphone app.















