10/25/2022
PITTSBURGH – Black veterans hospitalized with COVID-19 were less likely to receive evidence-based treatments than their white counterparts but did not have higher rates of death or readmission, according to new research led by University of Pittsburgh School of Medicine physician-scientists that was published today in JAMA Network Open.
 The study, which examined two years of data from 130 Department of Veterans Affairs Medical Centers (VAMCs), found that the disparities in treatment were driven by differences in care that occurred within and between hospitals. In other words, individual hospitals were providing different rates of treatment to their Black and white patients, in addition to there being differences in care between hospitals that treat a disproportionate number of Black patients compared to those that treat mainly white patients.
The study, which examined two years of data from 130 Department of Veterans Affairs Medical Centers (VAMCs), found that the disparities in treatment were driven by differences in care that occurred within and between hospitals. In other words, individual hospitals were providing different rates of treatment to their Black and white patients, in addition to there being differences in care between hospitals that treat a disproportionate number of Black patients compared to those that treat mainly white patients.
“Our study goes beyond showing there is a problem with racial disparities in COVID-19 medical care,” said lead author Alexander Castro, a fourth-year medical student in Pitt’s School of Medicine. “We are pointing to where we need to concentrate our efforts to better understand why these racial disparities are occurring and how we can counteract them.”
The study looked at records from 48,222 veterans – 28.1% Black – who had been hospitalized with COVID-19 at a VAMC between March 1, 2020 and February 28, 2022. The patients were a median age of 72, and 94.2% were men.
Two-thirds of the patients who needed breathing support – either from oxygen or mechanical ventilation – received systemic steroids, such as dexamethasone, which started to be recommended in the fall of 2020 after a worldwide trial determined they improved the chances that very sick COVID-19 patients would survive. Black patients had 12% lower odds of receiving the drug than their white counterparts at the same VAMC hospital.
Similarly, Black patients were 11% less likely to receive the antiviral remdesivir, which is recommended for most adults hospitalized with COVID-19 within a week of symptom onset. And they were 23% less likely to receive an immunomodulatory drug, such as tocilizumab, which is recommended for moderately to severely ill hospitalized COVID-19 patients.
However, after adjusting for patient demographics, chronic health conditions, severity of illness and receipt of COVID-19 treatments, Black and white patients had similar outcomes when it came to their likelihood of dying in the hospital or being readmitted within 30 days.
The researchers said the lack of disparities in outcomes, despite disparities in treatment, needs further investigation and couldn’t be explained by their study.
 “We should not be seeing racial disparities in treatment, even if those disparities may not be resulting in more deaths,” said co-author Florian Mayr, M.D., M.P.H., assistant professor of critical care medicine in Pitt’s School of Medicine and intensivist at the VA Pittsburgh Healthcare System. “When entire hospitals are underperforming in providing evidence-based treatments, we can target hospital-wide interventions to address the problem. But correcting racial disparities in provision of treatment within hospitals requires a multilayer approach.”
“We should not be seeing racial disparities in treatment, even if those disparities may not be resulting in more deaths,” said co-author Florian Mayr, M.D., M.P.H., assistant professor of critical care medicine in Pitt’s School of Medicine and intensivist at the VA Pittsburgh Healthcare System. “When entire hospitals are underperforming in providing evidence-based treatments, we can target hospital-wide interventions to address the problem. But correcting racial disparities in provision of treatment within hospitals requires a multilayer approach.”
Mayr said improvement efforts that could be considered include employing a more racially diverse mix of clinicians, which has been shown in studies to improve the quality of care; boots-on-the-ground surveying of physicians to better understand their treatment decisions; and investigating whether devices like thermometers and pulse-oximeters, which studies have shown are racially biased toward those with darker skin, could be interfering with treatment decisions.
In addition, the VAMCs require clinicians to get consent to use various COVID-19 treatments before administering them. Distrust in the medical community could be biasing consent for treatment and driving some of the disparities, Mayr said.
The team noted that their study population was largely dominated by older men, so their results shouldn’t be extrapolated to hospitals that treat a younger population that includes more women, though those hospitals can use the study to prompt their own investigations.
“COVID-19 treatments are not the only example of racial disparities in care,” said Castro. “It’s happening in sepsis, pneumonia and hospital-acquired infections, among other measures. It is a multifaceted issue without easy solutions, making it one of the most difficult – and most important – questions facing clinical research.”
Adeel A. Butt, M.B.B.S., M.S., of the VA Pittsburgh Healthcare System and Weill Cornell Medicine, is senior author of this research. Additional authors are Victor Talisa, Ph.D., Obaid S. Shaikh, M.D., and Sachin Yende, M.D., M.S., all of the VA Pittsburgh Healthcare System and Pitt; and Saad B. Omer, M.B.B.S., Ph.D., of Yale University.
This research was supported by National Institutes of Health grant K23GM132688 and VA Health Services Research and Development Service grant RES 13-457.
Top right photo:
PHOTO DETAILS: (click images for high-res versions)
CAPTION: Alexander Castro
CREDIT: Alexander Castro
Middle center photo:
PHOTO DETAILS: (click images for high-res versions)
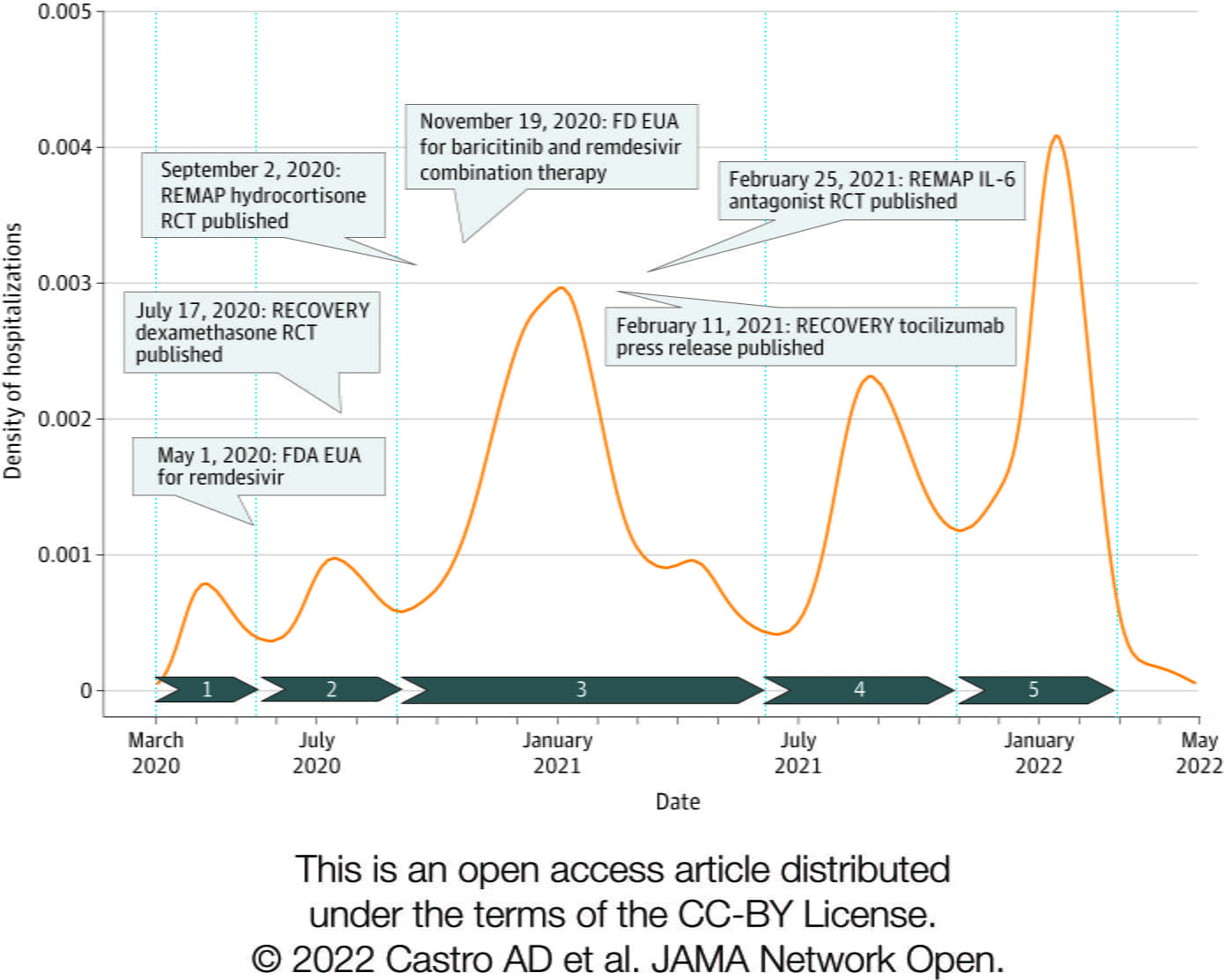
CAPTION: COVID-19 waves and treatments. This graphic shows COVID-19 hospitalization peaks across the first two years of the pandemic, indicating when evidence for the validity of new treatments became available.
CREDIT: Castro, A.D., et al., (2022) JAMA Network Open
Bottom right photo:
PHOTO DETAILS: (click images for high-res versions)
CAPTION: Florian Mayr, M.D., M.P.H.
CREDIT: University of Pittsburgh