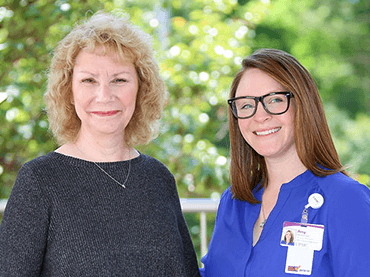
Like so many others, Diane was suffering in silence. Although she dedicating her life to helping others, she also valued her privacy—but everything changed when she met Amy Vandermark, a pelvic floor rehabilitation specialist at UPMC.
Through her decade-long column, “Life’s Changes,” in the Williamsport Sun Gazette and monthly workshop “Navigating Life Changes,” Diane has made it her mission to help people navigate life’s many changes.
While researching speakers for her workshop, Diane met Amy, a physical therapist and pelvic floor rehabilitation specialist at UPMC.
Like Diane, Amy shares a passion for impacting lives in a positive way. What neither woman could have predicted was how attending the pelvic pain support group at UPMC Muncy would change Diane’s life.
After hearing Amy speak, Diane realized the symptoms she’d been experiencing for years could be pelvic pain—a reaction all too common.
“Many of the people we see in physical therapy for pelvic rehabilitation have been to several physicians to find an answer,” explains Amy. “Many times, pelvic floor disorder goes undiagnosed.”
What is Pelvic Floor Disorder?
The National Institute of Child Health and Human Development estimates one-third of women in the U.S. suffer from a form of pelvic floor disorder, but it can also affect men and children. It is estimated nearly 61 percent of those with chronic pelvic pain have no diagnosis. Chronic pelvic pain is defined as any pain or burning lasting longer than six months in the lower abdomen, genitals, vagina, perineum, anus, or lower back.
Common pelvic floor disorders include:
- Chronic pelvic pain
- Constipation
- Incontinence
- Urinary urgency (retention, and frequency)
- Pelvic organ prolapse
- Painful bladder syndrome
- Pelvic pain after cancer or surgery
The Hidden Secret of Pelvic Pain
Many patients with pelvic pain go untreated because they don’t realize treatment is available. Diane had been suffering from pelvic pain for decades.
“It was something I learned to live with, yet was hopeful to find relief someday,” notes Diane.
Diane went to her primary care physician, Thomas Wallace, MD, to discuss her symptoms and talk about a referral for physical therapy. He referred her to OB/GYN, Natasha Alligood-Percoco, MD, to rule out any other medical issues. She determined Diane needed surgery and referred her to Amy for therapy to aid in pre- and post-surgical treatment.
Diane’s Journey in Healing
At their first appointment, Amy and Diane met in a private treatment room to discuss her medical history, symptoms, and personal goals.
“We do a comprehensive evaluation at the first appointment including posture, alignment, range of motion, mobility, and muscle function of the hip and pelvis,” Amy explains. “We do an internal pelvic floor muscle examination and use biofeedback if needed to test strength, tone, and sensation of the pelvic floor muscles.”
Diane was immediately put at ease, “Amy is thoughtful with her questions, and has kindness and compassion that parallels her professionalism. She recognized it was difficult for me to open up, and I didn’t always have the words to describe what was going on in my body. I was able to open up because I recognized she was truly trying to help me.”
Amy developed an individualized treatment program, including exercises and relaxation techniques, to treat the pain and relax the pelvic floor.
Diane and Amy Remain Focused on Helping Others
Through this experience, Amy and Diane discovered a shared passion for helping others and became close friends, partnering to educate their community that help is possible.
Diane says, “My life is about educating people to be more involved, more authentic, and give themselves more self-care. If sharing my story and supporting Amy’s amazing work at UPMC, helps anyone in their own healing journey, I will be grateful.”
Both women recommend everyone be more open with their doctor.
“Women and men should share their personal challenges with their doctor and ask questions,” advises Amy. “If you are experiencing any pelvic disorders, ask your doctor if you may benefit from pelvic floor rehabilitation.”