On this page:
What Are Benign Breast Conditions?
Doctors define benign breast conditions as noncancerous issues of the breasts. Although they may warrant medical evaluation and be uncomfortable or even painful, they're not considered life-threatening.
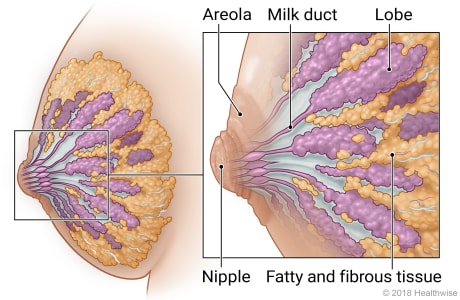
Anatomy of the female breast
The lobes, milk ducts, areola, nipple, and fatty and fibrous tissue are the main parts of the female breast.
Fat and fibrous tissue make up most of the breast. The lobes and ducts are spread throughout this tissue. Sometimes breast tissue is "dense." This means there is more fibrous tissue than fat.
At childbirth, the lobes produce milk. The milk flows through the milk ducts to the nipple. Around the nipple is the areola. It contains tiny glands that lubricate the nipple during breastfeeding. The areola also contains smooth muscles that cause the nipple to push out. This makes it easier for a baby to latch on during breastfeeding.
© 2016-2025 Healthwise, Incorporated. This information does not replace the advice of a doctor.
What are the most common types of benign breast conditions?
The most common types of benign breast disease include:
Abscess
A collection of pus can sometimes form in conjunction with mastitis (an infection of a breast gland). Antibiotics can treat mastitis, and breast imagers (radiologists) or surgeons may aspirate or drain the abscess.
Mastitis
Breast mastitis is an infection that develops in the breast. It may cause swelling and increased blood flow, and your breast may become painful, red, and warm to the touch.
Mastitis is typically treated with antibiotics. But if antibiotics don't improve your condition, your doctor may suggest testing for inflammatory breast cancer, which is rare but can mimic some symptoms of mastitis.
Nipple discharge
Clear, green, or milky discharge is unlikely to be cancerous. However, if the discharge is red or red-brown, suggesting it contains blood, it could be cancer and should be checked.
The most common cause of nipple discharge is physiologic, meaning normal glandular fluid production. Other causes of nipple discharge are injury, infection, or benign tumors. Collected fluid can be reviewed under a microscope to check for the presence of cancer cells.
Duct ectasia
Mammary duct ectasia occurs when a milk duct dilates (enlarges), causing inflammation and thickening. It may affect one or both breasts. Some people have pain or nipple discharge, but many have no symptoms at all.
Fibroadenoma
Fibroadenomas are benign tumors in the breast. More than 25% (one in four) women have fibroadenomas. They're the most common benign breast condition and often don't need treatment.
Fibroadenomas can be distinguished from cancerous lumps by how easily they move around inside the breast and their clearly defined edges, as seen on imaging.
Fibrosis and simple cysts
Many breast lumps turn out to be benign changes in fibrous tissue (fibrosis), cysts, or both. These are known as fibrocystic changes.
Formerly called fibrocystic disease, the term was changed when it was recognized as a normal finding in many women. Fibrocystic changes are most common in women of childbearing age, but they can affect women of any age.
Hyperplasia
Hyperplasia is an overgrowth of the cells that line the breast's ducts (small tubes) or lobules (milk-producing glands). Although not cancer, some types of hyperplasia may be related to an increased risk of developing breast cancer.
Lobular carcinoma in situ (LCIS)
Lobular carcinoma in situ (LCIS) may be seen on a breast biopsy. In LCIS, cells that look like cancer cells grow in the lining of lobules but don’t break through the wall of the lobules. LCIS does not become invasive breast cancer, but it may put a person at increased risk of developing breast cancer later in life.
Intraductal papillomas
Intraductal papillomas are wart-like tumors that grow within the breasts’ milk ducts. They are fibrovascular tumors made up of gland tissue, fibrous tissue, and blood vessels.
Fat necrosis and oil cysts
Fat necrosis is the result of an area of fatty breast tissue that has died, often following trauma. As the fat cells die, they release their contents in the form of small sacs of fluid called oil cysts.
The condition can develop after an injury, breast surgery, or radiation treatment. Over time, small calcium deposits can form around the cysts, which may make them visible on a mammogram.
What are the least common types of benign breast conditions?
Other less common benign breast diseases we treat include:
Phyllodes tumors
Phyllodes tumors are large, fast-growing tumors that form in the connective tissues of the breast — not in the ducts or glands, where most breast cancers start. They're most common in women in their 40s but may affect women of any age. Although most phyllodes tumors are benign, a small number may be malignant (cancerous).
Radial scars
Also called complex sclerosing lesions, radial scars are most often found on a breast biopsy done for another purpose. They sometimes show up on a mammogram as a distortion of normal breast tissue.
Although they're not really scars, they look like scars under a microscope. They don’t usually cause symptoms and may slightly increase your risk of developing breast cancer.
More breast changes that aren't cancer include:
- Adenomyoepithelioma — A very rare tumor formed by certain cells in the walls of the milk ducts.
- Granular cell tumor — A tumor that begins in early forms of Schwann cells, which normally surround and help insulate nerve cells. They rarely occur in the breast.
- Hamartoma — A smooth, painless lump formed by the overgrowth of mature breast cells, which can be made up of fatty, fibrous, and gland tissues.
- Hemangioma — A rare tumor made up of blood vessels.
- Hematoma — A collection of blood within the breast caused by internal bleeding, such as bruising.
- Lipoma — A fatty tumor that can appear almost anywhere in the body, including the breast. It usually isn't painful.
- Neurofibroma — A tumor that’s an overgrowth of nerve cells.
Back to top
What Are the Signs and Symptoms of Benign Breast Conditions?
Some benign breast changes may have no signs or symptoms.
The most common symptoms are:
- Breast lumps.
- Changes in breast size or shape.
- Changes in skin color or texture.
- Nipple discharge.
- Nipple inversion.
- Pain.
Other issues might be found on a mammogram. Whether you’re having symptoms or not, benign breast disease can be hard to tell apart from breast cancer. More exams or tests might be needed to find out for sure.
Back to top
How Do You Diagnose Benign Breast Conditions?
To diagnose benign breast conditions, your doctor may perform a physical examination of your breasts and order additional tests to confirm the diagnosis.
Tests to diagnose benign breast conditions
Diagnostic mammography exams are usually the first tests ordered when there are signs and symptoms of breast disease. (This test also may be done if you're asked to return for more evaluation after a screening mammography exam.) You need a prescription for diagnostic mammography.
After the diagnostic mammogram:
- You may have other tests, such as breast ultrasound or digital breast tomosynthesis (3D mammography), if needed.
- Your exam results will be given to you that day before you leave.
- The radiologist may ask for a breast biopsy if more information is needed based on the mammography (and ultrasound) findings. Based on the biopsy results, the radiologist may recommend that you return for annual screening or diagnostic mammograms.
Back to top
How Do You Treat Benign Breast Conditions?
No treatment is usually needed for most benign breast conditions, especially ones that pose no increase or only a slight increase in cancer risk. You should continue routine screening with mammograms and gynecological visits.
Medication for benign breast conditions
If you have an infection, like mastitis, your doctor may prescribe antibiotics.
Surgery for benign breast conditions
Most benign breast conditions do not require surgery. However, if your doctor recommends surgical removal of a growth or abscess, they may also recommend a follow-up breast exam and imaging tests within six to 12 months.
Watchful waiting for benign breast conditions
If you have a cyst, fibroadenoma, or other growth that wasn’t removed, your doctor may recommend watching it with breast screenings and ultrasounds for a few years. Alternatively, your provider may have you go back to annual screenings.
If you have a benign condition posing a moderate risk of breast cancer, you may need closer follow-up. Examples include atypical hyperplasia or lobular carcinoma in situ.
If you have a benign breast condition that poses a slight increase in breast cancer risk, and you also have known breast cancer risk factors, such as family history, you can work with your provider to understand your risk and plan what’s right for you. You also may want to see a breast specialist with expertise in benign breast conditions.
Back to top
By UPMC Editorial Staff. Last reviewed on 2025-09-18.