What Is A Lumpectomy?
A lumpectomy — also known as breast-conserving surgery or a partial mastectomy — is a surgical procedure to remove a breast tumor while sparing as much healthy breast tissue as possible.
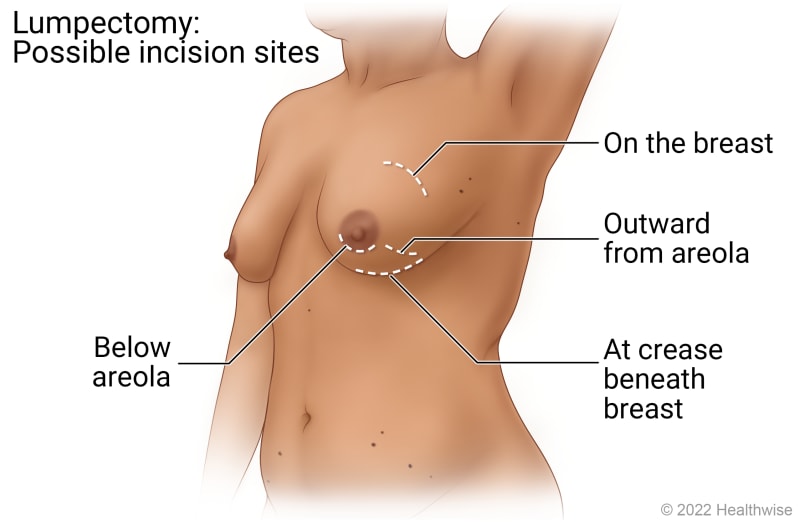
Lumpectomy is surgery to remove a tumor in the breast. The cut (incision) is made close to the tumor. Common places include on the breast, beneath the breast, and near the areola.
© 2016-2025 Healthwise, Incorporated. This information does not replace the advice of a doctor.
Hidden Scar™ surgery
UPMC is one of only two Centers of Excellence for Hidden Scar™ surgery in Pennsylvania. Hidden Scar breast cancer surgery is an advanced technique that allows breast surgeons to remove cancerous tissue through a single incision in an inconspicuous area to minimize visible scarring. In many cases, hidden scar surgery allows surgeons to preserve a natural-looking breast by sparing the nipple, areola, and surrounding tissue.
Hidden Scar breast cancer surgery may be appropriate if you are a candidate for a nipple sparing mastectomy or a breast-conserving (lumpectomy) procedure.
Conditions we treat with lumpectomy procedures
Why Would I Need A Lumpectomy?
You may need a lumpectomy if you are diagnosed with early-stage breast cancer, have an average risk of breast cancer recurrence, and do not want to undergo a mastectomy procedure to remove your entire breast.
Who’s a candidate for lumpectomy?
You may be a candidate for a lumpectomy procedure if:
- You are at average risk for breast cancer recurrence.
- You are diagnosed with early-stage breast cancer.
- You are willing to have radiation therapy or other medical oncology treatments after your lumpectomy procedure to kill any remaining cancer cells.
Alternatives to lumpectomy procedures`
What Are the Risks and Complications of Lumpectomy Procedures?
Like all surgical procedures, lumpectomy comes with some risks, including:
- A change in the shape of your breast.
- Hematoma (collection of blood) or seroma (fluid) in your wound.
- Infection at your surgical site.
- Lymphedema, which may cause swelling in your arm after lymph nodes are removed.
- Nerve damage that causes numbness or pain.
- Pain, swelling, and tenderness at your surgical site.
- Scar tissue or a dimple at your surgical site.
What Should I Expect From A Lumpectomy?
Before: How to prepare for a lumpectomy
To prepare for the procedure, you should:
- Fast for a certain period of time prior to the procedure. Your doctor will inform you if you need to fast and, if so, how long to fast (typically overnight).
- Have any tests that your doctor recommends. For example, your doctor may request a blood test before the procedure to determine how long it takes your blood to clot.
- Tell your doctor if you are sensitive or allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
- Tell your doctor about all medications (prescription and over-the-counter) and herbal or other supplements you are taking.
- Tell your doctor if you have any other health conditions. Your care team may need to take certain precautions during your procedure for your safety.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any blood-thinning medications, aspirin, or other medications that affect blood clotting. You may need to stop some of the medications prior to the procedure.
- Tell your doctor if you are breastfeeding, pregnant, or think you might be pregnant.
On the day of your procedure, please bring your photo ID and health insurance card(s). Leave valuables such as cash and jewelry at home.
You may be discharged the same day as your surgery, or you may need to stay in the hospital overnight. Your doctor will let you know what to expect.
If you need to stay overnight, please bring the following essentials: toiletries, a robe, slippers, a cell phone and charger, medications, and a change of clothes. You will also need to arrange for someone to drive you home after you are discharged.
Presurgical localization procedures
Before your lumpectomy, your doctor may perform a localization procedure so they can precisely remove your breast tumor if it can’t be easily felt or seen.
Localization procedures include:
- Radioactive seed localization — A radioactive seed that is about the size of a grain of rice is placed in the center of your tumor a few days before your surgery. During your procedure, your surgeons will use a special tool to locate the seed so they can precisely remove your tumor.
- Needle localization — Also known as fine wire localization, needle localization uses ultrasound, MRI, or mammography imaging guidance and a small needle to place a thin wire that marks the location of a suspicious mass in your breast.
How long does a lumpectomy procedure take?
Lumpectomy procedures typically take 30 to 90 minutes. If you are having immediate reconstructive surgery, your procedure may take longer.
During your lumpectomy
When you arrive at the hospital, you will meet with your care team for final preparations.
You will receive an IV in your hand or arm. You will have general anesthesia to put you to sleep.
During your lumpectomy, your surgeon will:
- Locate your tumor using a marker placed before surgery, if applicable.
- Remove your breast tumor. Your surgeon may also remove lymph nodes from your underarm area.
- Send your tumor and a margin of surrounding tissue, as well as any lymph nodes that were removed, to the lab to be tested for cancer.
- Place a small clip to mark the area where your tumor was removed so your radiation oncologist knows which area to treat.
- Perform immediate reconstructive surgery to restore the shape and appearance of your breast or prepare your breast for future reconstructive surgery.
- Close your incision and cover it with a bandage.
Recovery after lumpectomy
After your procedure is complete, you will be monitored in the recovery area. Most people are discharged the same day. You will need to arrange for someone to drive you home from the hospital.
You may have bleeding, bruising, or swelling that will go away in a few weeks. You may also have scarring or notice a change in the shape of your breast.
During your recovery, you should:
- Ask your doctor if it is safe for you to take acetaminophen to manage mild pain or discomfort.
- Apply ice to your breast for 15 to 20 minutes every two hours for the first 24 hours after your procedure to reduce bruising and swelling. Switch to warm compresses after 48 hours to manage any discomfort.
- Wear a sports bra for the first few days after your procedure.
- Keep your bandage dry and leave it in place for 24 hours after your procedure. Do not allow your procedure site to get wet for 24 hours after your procedure.
- Avoid strenuous activity for several days after your procedure, including activities that require pushing, pulling, or lifting more than 10 pounds.
- Ask your doctor when it is safe to resume taking blood-thinning medications, if applicable.
Additional treatment after lumpectomy
Your breast cancer care team may recommend additional radiation therapy or medical oncology treatments after your lumpectomy. These treatments may be used to kill any remaining cancer cells and reduce your risk of cancer recurrence.
When to call your doctor about complications
Call your doctor right away if you notice signs of infection or complications, including:
- Excessive bleeding.
- Drainage from your incision site.
- Pressure.
- Redness.
- Swelling.
- Warmth.
What is the recovery time after a lumpectomy?
Most people can return to their normal activities within one to two weeks after a lumpectomy.
What’s the prognosis after lumpectomy?
Your prognosis after lumpectomy depends on the type and stage of your cancer, as well as your overall health. Generally, people with early-stage breast cancer that has not spread beyond the breast have higher survival rates than those with late-stage breast cancer that has spread to the lymph nodes or other areas of the body. Your doctor will discuss your prognosis with you.
What’s the success rate of lumpectomy?
Lumpectomy is a highly successful procedure for treating some types of small, early-stage breast tumors. Your doctor will discuss the expected success rate of your procedure with you.
Why Choose UPMC for lumpectomy surgery?
When you choose UPMC for lumpectomy surgery, you will receive:
- A full range of breast surgery options — Your care team will recommend the appropriate surgical procedure for your type of breast cancer while considering your lifestyle, preferences, and reconstruction goals.
- Collaborative, multidisciplinary care — Your breast cancer care team will work closely with our plastic and reconstructive breast surgeons to provide the best cancer treatment and cosmetic results.
- Supportive services — Your team will encourage you to play an active role in your breast cancer treatment plan and provide the support you need to manage your treatment and recovery.
By UPMC Editorial Staff. Last reviewed on 2025-09-18.