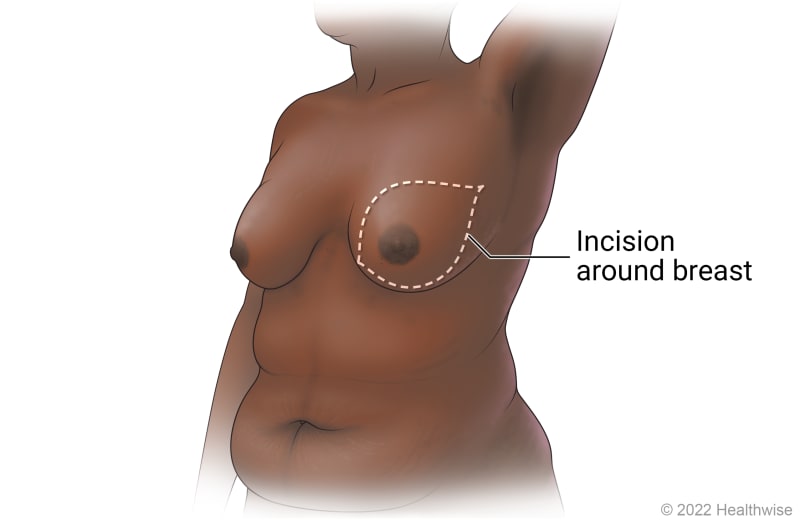
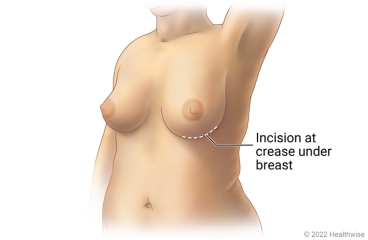
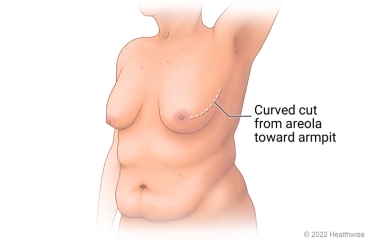
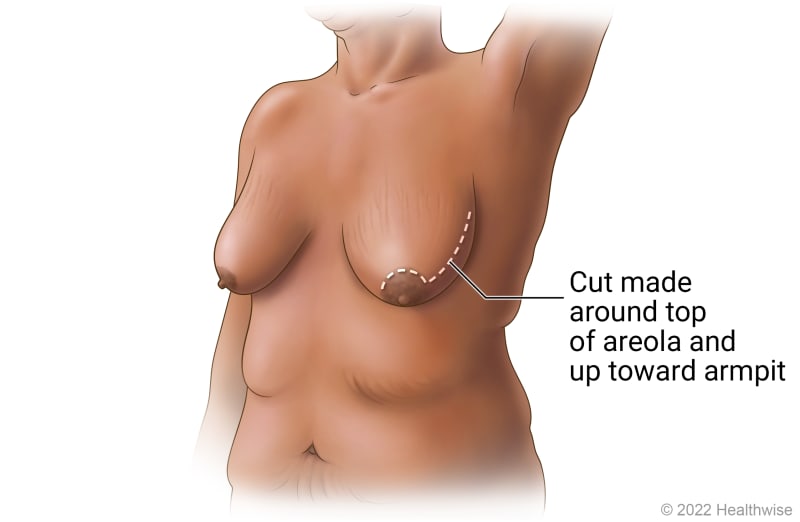
Hidden Scar™ surgery
UPMC is one of only two Centers of Excellence for Hidden Scar surgery in Pennsylvania.
Hidden scar breast cancer surgery is an advanced technique that allows breast surgeons to remove cancerous tissue through a single incision in an inconspicuous area to minimize visible scarring. In many cases, hidden scar surgery allows surgeons to preserve a natural-looking breast by sparing the nipple, areola, and surrounding tissue.
This surgery may be appropriate if you are a candidate for a nipple-sparing mastectomy or breast-conserving lumpectomy procedure. Qualification depends on tumor size and location, as well as breast shape and size.
Conditions we treat with mastectomy
Mastectomy is a procedure to treat or prevent breast cancer.
Why Would I Need A Mastectomy?
You may need a mastectomy if you are diagnosed with breast cancer and you:
- Are not a candidate for breast-conserving surgery (lumpectomy).
- Choose to have a mastectomy instead of a lumpectomy to reduce recurrence risk.
A double mastectomy also may be a preventive treatment option for women at very high risk of developing breast cancer.
Who’s a candidate for a mastectomy?
You may be a candidate for a mastectomy if you are diagnosed with breast cancer that cannot be treated with breast-conserving surgery. You may also be a candidate for a preventive (prophylactic or risk-reducing) mastectomy if you have a gene mutation that puts you at very high risk of developing breast cancer in the future, or if you are at high risk of breast cancer recurrence after your initial treatment.
How does a mastectomy reduce cancer risk?
A mastectomy may reduce your risk of developing breast cancer by removing breast tissue where cancer cells may develop. In some cases, it can reduce the risk of developing breast cancer by up to 90%.
Alternatives to mastectomy
What Are the Risks and Complications of Mastectomy?
Like all surgical procedures, mastectomy comes with some risks, including:
- A hematoma (collection of blood) or seroma (fluid) in your wound.
- Flap necrosis, which occurs when tissue dies due to a lack of blood supply.
- Infection at your surgical site.
- Lymphedema, which may cause swelling in your arm after lymph nodes are removed.
- Pain, swelling, and tenderness at your surgical site.
- Post-mastectomy pain syndrome (PMPS), which is due to nerve damage that leads to numbness or pain.
- Reduced range of motion in your arm or shoulder.
What Should I Expect From A Mastectomy?
Before: How to prepare for a mastectomy
To prepare for the procedure, you should:
- Fast for a certain period of time prior to the procedure. Your doctor will inform you if you need to fast and, if so, how long to fast (typically overnight).
- Have any tests that your doctor recommends. For example, your doctor may request a blood test before the procedure to determine how long it takes your blood to clot.
- Tell your doctor if you are sensitive or allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
- Tell your doctor about all medications (prescription and over-the-counter) and herbal or other supplements you are taking.
- Tell your doctor if you have any other health conditions. Your care team may need to take certain precautions during your procedure for your safety.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any blood-thinning medications, aspirin, or other medications that affect blood clotting. You may need to stop some of the medications prior to the procedure.
- Tell your doctor if you are breastfeeding, pregnant, or think you might be pregnant.
On the day of your procedure, please bring your photo ID and health insurance card(s). Leave valuables like cash and jewelry at home.
You may be discharged the same day as your surgery, or you may need to stay in the hospital overnight. Your doctor will let you know what to expect.
If you need to stay overnight, you should bring toiletries, a robe, slippers, a cell phone and charger, medications, and a change of clothes. You will also need to arrange for someone to drive you home after you are discharged.
How long does a mastectomy take?
The length of your mastectomy procedure depends on the type of procedure you are having. A simple mastectomy typically takes one to three hours, and a double mastectomy takes four to six hours. If you are having an immediate reconstruction procedure, your surgery could take three to six hours or longer.
During your mastectomy
When you arrive at the hospital, you will meet with your care team for final preparations.
You will receive an IV in your hand or arm. You will have general anesthesia to put you to sleep.
During your mastectomy, your surgeon will:
- Remove your breast tissue. Depending on the type of mastectomy you are having, your surgeon may also remove lymph nodes from your underarm area or other tissue.
- Perform an immediate reconstruction or prepare your breast for a delayed reconstruction procedure, if desired.
- Place a surgical drain to remove excess fluid from the surgical site.
- Close your incision and cover it with a bandage.
Recovery after mastectomy
After your procedure is complete, you will be monitored in the recovery area. If you are staying overnight in the hospital, you will be transferred to your room. If you are discharged the same day, you will be released from the hospital when your condition is stable. Whether you stay overnight or are discharged the same day, you will need to arrange for someone to drive you home from the hospital.
Before you go home, your doctor will tell you:
- How to care for your wounds and watch for signs of infection or complications.
- What medications you need to take.
- When to call your doctor or 911 if you have certain symptoms.
- When you should schedule your follow-up appointment, if one has not been scheduled already.
- When you can return to your normal activities, such as driving and bathing.
If your lymph nodes were removed as part of your mastectomy, your doctor may also recommend that you see a lymphedema specialist. The lymphedema specialist can monitor your condition and help you reduce your risk of lymphedema after your procedure.
Additional treatment after mastectomy
Your breast cancer care team may recommend radiation therapy or medical oncology treatments after your mastectomy. These treatments may be used to kill any remaining cancer cells or reduce your risk of cancer recurrence.
When to call your doctor about complications
You should let your surgeon know if you have:
- A fever of more than 100.0°F.
- Difficulty breathing.
- Pain, redness, bleeding, drainage, or increased swelling at your treatment site.
- Severe pain that does not respond to medication.
- Swelling in your arm or hand.
What’s the prognosis after mastectomy?
Your prognosis after mastectomy depends on the type and stage of your cancer, as well as your overall health. Generally, people with early-stage breast cancer that has not spread beyond the breast have higher survival rates than those with late-stage breast cancer that has spread to the lymph nodes or other areas of the body. Your doctor will discuss your prognosis with you.
What’s the success rate of mastectomy?
Mastectomy is a highly successful procedure for treating breast cancer. It is also an effective preventive treatment to reduce the risk of developing breast cancer in the future.
Why Choose UPMC for Mastectomy Surgery?
When you choose UPMC for mastectomy surgery, you will receive:
- A full range of breast surgery options — Your care team will recommend the appropriate surgical procedure for your type of breast cancer while considering your lifestyle, preferences, and reconstruction goals.
- Collaborative, multidisciplinary care — Your breast cancer care team will work closely with our plastic and reconstructive breast surgeons to provide the best cancer treatment and cosmetic results.
- Supportive services — Your team will encourage you to play an active role in your breast cancer treatment plan and provide the support you need to manage your treatment and recovery.
By UPMC Editorial Staff. Last reviewed on 2025-09-18.