What Is Liver Transplant Surgery?
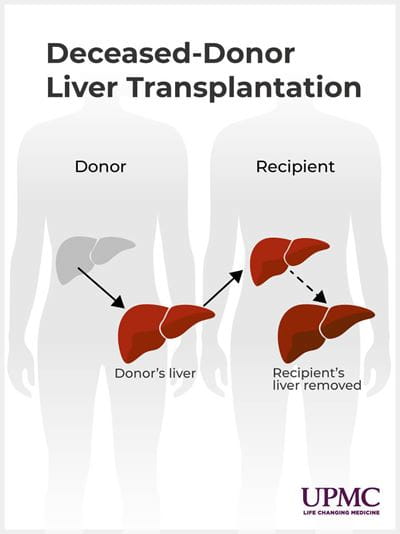
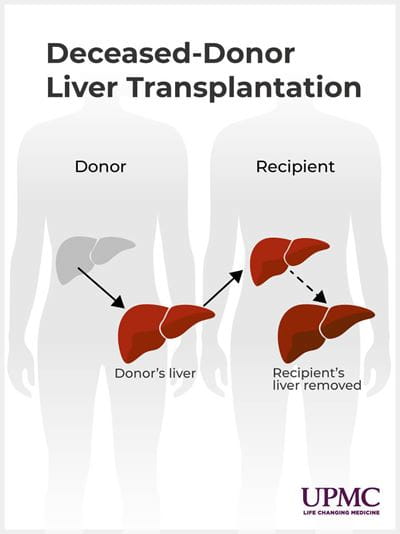
During a liver transplant, a surgeon removes your diseased liver and replaces it with a liver from a deceased donor or a portion of a healthy adult’s liver (living-donor liver transplant).
In living-donor transplants, the liver has the unique ability to regenerate, or regrow, in just a few months, leaving both the living donor and the recipient with a fully functioning liver.
Types of liver transplant surgery
Our liver transplant experts perform several types of liver transplant surgeries, including:
Liver transplantation
UPMC provides complete liver transplantation care for people with complex liver conditions, including those with advanced liver cancer. Liver transplant surgeons are experienced in using both deceased donor livers and portions of healthy adult livers (living-donor liver transplant).
Living-donor liver transplantation
At UPMC, we discuss living donation with every patient, as it can reduce wait times from years to just months while also improving outcomes.
UPMC provides living-donor liver transplant services to all who will benefit, including patients with complex conditions, such as:
- Acute liver failure.
- Alcohol-associated liver disease.
- Cholangiocarcinoma.
- Low MELD score.
Living-donor liver transplant for liver cancer
UPMC’s expertise and innovation includes transplant oncology — a treatment option in which doctors remove a patient’s cancerous liver and replace it with part of a living donor’s healthy liver.
The donated liver portion regrows to its original size, usually a few months after transplant. The donor’s liver regrows as well. A living-donor liver transplant can be an earlier and faster treatment for patients with advanced cancers.
UPMC offers living-donor liver transplantation as a treatment option for patients with cancer diagnoses, including:
- Hepatocellular carcinoma (HCC).
- Hilar cholangiocarcinoma.
- Intrahepatic cholangiocarcinoma or mixed cholangio/hepatocellular carcinoma.
- Unresectable metastatic colorectal cancer.
- Unresectable neuroendocrine tumor.
Liver resection for cancer
Liver resection involves the total or partial removal of the liver. Because of its regenerative ability, liver resection allows for continual functionality, even when parts of it are removed.
For people diagnosed with liver cancer, liver resection offers the best chance for long-term survival. Our team has extensive experience in minimally invasive (laparoscopic) liver surgery as well as traditional (open) liver surgery.
Bile duct reconstruction
Bile duct cancer is cancer in the tubes that carry bile from the liver to the gallbladder. Bile is the fluid your liver makes and uses to digest fats in the food you eat.
At UPMC, our transplant team conducts different surgeries to treat bile duct cancer, such as:
- Bile duct removal — To remove the bile duct if the cancer hasn't spread.
- Liver transplant — To remove the diseased liver and replace it with a healthy liver from a living donor.
- Partial hepatectomy — To remove the tumor and some of the surrounding tissue, leaving healthy tissue intact.
Surgical and nonsurgical treatment for portal hypertension and variceal bleeding
Portal hypertension is the increased pressure in the portal vein, which is often a symptom of liver disease that is commonly caused by scarring in the liver. Similarly, variceal bleeding is initiated when there is too much pressure on the portal vein, causing blood flow to be restricted or pushed backward.
At UPMC, depending on the complexity of the disease, we offer treatment options such as liver transplantation and antiviral medications — the same ones used to treat hepatitis B and hepatitis C.
Conditions we treat with liver transplant surgery
- Acute liver failure.
- Alcohol-associated hepatitis.
- Bile duct cancer.
- Cholangiocarcinoma.
- Hepatocellular carcinoma (HCC).
- Hilar cholangiocarcinoma.
- Intrahepatic cholangiocarcinoma or mixed cholangio/hepatocellular carcinoma.
- Low MELD score.
- Portal hypertension.
- Unresectable metastatic colorectal cancer.
- Unresectable neuroendocrine tumor.
- Variceal bleeding.
Why Would I Need Liver Transplant Surgery?
You may need liver transplant surgery if you have end-stage liver disease that can no longer be treated with medical therapy.
Who’s a candidate for liver transplant surgery?
You may be a candidate for liver transplant surgery if you have end-stage liver disease caused by:
- A failed prior liver transplant.
- Acute liver disease from toxins, including acetaminophen.
- Alcohol-associated liver disease.
- Alpha 1 antitrypsin deficiency.
- Autoimmune hepatitis.
- Hemochromatosis.
- Hepatitis B.
- Hepatitis C.
- Metabolic dysfunction-associated steatotic liver disease (MASLD).
- Polycystic disease.
- Primary biliary cirrhosis.
- Primary liver cancers.
- Primary sclerosing cholangitis.
- Veno-occlusive disease.
- Wilson's disease.
Who is not a candidate for liver transplant surgery?
Our team makes every attempt to ensure that people chosen for transplant evaluation are the most suitable for the surgery. There are many requirements for liver transplant surgery.
Before you can begin the liver transplant evaluation process, you may not have:
- Active infections.
- Abused substances such as alcohol, nicotine, marijuana, cocaine, heroin, or other illicit substances for at least six months.
- Cancer outside the liver.
- A severe, untreated psychiatric disorder.
- An inability or unwillingness to follow your pre- or posttransplant treatment plan.
- Lack of adequate social support.
- Lack of adequate insurance.
- Other diseases or conditions.
You must also be willing and able to make lifestyle changes and follow your pre- and posttransplant treatment plan.
Who is a candidate for living-donor liver transplant surgery?
At UPMC, we believe that living-donor liver transplant is a first-line option for liver transplant candidates, not a last resort.
Our team will work with you to determine if living-donor liver transplant is right for you. We will help find a suitable living donor and guide you and your donor through the living organ donation process.
What Are the Risks and Complications of Liver Transplant Surgery?
Although many liver transplants occur with little to no problems, there are some risks, including:
- Biliary complications.
- Bleeding.
- Infection.
- Primary graft dysfunction — (when the liver does not function right away).
- Rejection of the donor liver.
These complications can lead to:
- Increased recovery time.
- Longer hospital stays.
- Death, in severe cases.
UPMC uses innovative surgical methods and medications to help prevent or quickly respond to any complications from liver transplant surgery.
What Should I Expect From Liver Transplant Surgery?
At UPMC, your transplant team will guide you through every step of the treatment and liver transplant process.
The first step in the process is for your doctor to refer you for liver transplant services. We also accept self-referrals.
We will need your medical records and health information. We will also need your health insurance information so we can check your benefits and discuss the costs of transplantation.
For more information on what is needed to be referred, please visit the liver transplant referral checklist. Patient information can be faxed to 412-647-5070.
Patient information review
After the UPMC liver transplant team receives your medical records and information:
- A pretransplant nurse coordinator will collect and coordinate your outside medical, demographic, and financial information.
- The liver transplant team will review the information to determine if a transplant evaluation is appropriate.
- If a transplant evaluation is appropriate, we will obtain insurance authorization and contact you to schedule the evaluation.
Second opinions at UPMC
We routinely provide liver transplant care to those with complex cases and discuss the benefits of living-donor liver transplant with all patients who may qualify. If you’ve been turned down for a liver transplant at another center, or if you’d like a second opinion about your liver transplant options, our experts are available.
To learn more about receiving a second opinion at UPMC, call
412-647-5800.
Liver transplant evaluation
Evaluations for liver transplant help our liver transplant team understand your medical condition and decide whether a liver transplant would be in your best interest.
The outpatient transplant evaluation can take up to a week to complete. You are required to bring a care partner with you to each appointment. This person must meet with the transplant team and understand his or her role before, during, and after your liver transplant.
During your pre-liver transplant assessment, you might have these clinical tests:
- Blood tests.
- Consults and exams.
- Diagnostic tests.
- Imaging scans.
- Radiology tests.
We'll provide ongoing education about your surgery and send you a binder with a complete testing schedule, preparation instructions, and details about the liver transplant evaluation process.
Where can I schedule my liver transplant evaluation at UPMC?
UPMC has clinics throughout Pennsylvania where you can find out if a liver transplant is an option. Find a location.
Liver transplant evaluation tests
To prepare for certain tests, we may ask you not to eat or take certain medications before coming to the hospital. Any additional requirements for your pre-liver transplant evaluation will be on your schedule in the binder sent to you.
Your care team will give you instructions before each test and consultation.
Liver transplant tests include:
These tests will provide comprehensive health information that the transplant team will use to assess the function of your liver and other body systems to determine if you are a candidate for transplant.
Whenever possible, the transplant team will look for other ways to treat your liver disease and avoid performing a liver transplant too early.
You may also need to go to counseling or rehab for alcohol, depending on the cause of your liver failure. If you have alcohol-associated liver disease, the transplant team can work with you to develop a personalized treatment plan to address your alcohol use.
Your liver transplant evaluation and care team
Your multidisciplinary liver transplant evaluation and care team will include:
- Behavioral health nurses or psychiatrists — Will assist you and your care partner in coping with the stresses associated with chronic disease and the transplant process. They will also assess any current psychiatric/behavioral health symptoms that are being treated or may need to be treated.
- Credit analysts — Will review your insurance coverage and benefits information. They will help you to understand your insurance policy and will be your point of contact for insurance changes. They will also explain any parts of the liver transplant process that insurance does not cover and suggest options to assist with those costs.
- Liver transplant nurse coordinator — Will introduce you to the transplant process and review your evaluation schedule. The visit will include a preliminary health screening, a review of your medication, and an overview of the transplant process. Your transplant nurse coordinator is here to answer any questions you may have.
- Liver transplant surgeons — Will assess your physical capability and risks for transplant. They will review your liver disease and the medical management of your diagnosis and address all treatment options available to see if a liver transplant is the best option for you.
- Living-donor transplant nurse coordinator — Will answer any questions you may have about living donation and the transplant waitlist process.
- Nutritionists — Will assess your nutritional status, dietary knowledge, and provide education and recommendations for your diet.
- Pharmacists — Will meet with you to get a complete list of all your medicines and supplements you take, both prescription and over the counter, and ask you how you take your medicines.
- Social workers — Will discuss your support team at home, your prescription insurance coverage, and other social aspects of the transplant process. You will also learn about fundraising options.
- Transplant hepatologist — Will examine you, perform a medical history and physical, and focus on the signs and symptoms of your liver disease. They may also review other options for managing your liver disease.
What happens after my liver transplant evaluation?
Your multidisciplinary team will review your case at a selection meeting and decide whether a liver transplant is in your best interest. We will notify you of our decision within one week of the committee’s decision.
For those patients not approved for liver transplantation, our transplant team can make a referral for liver care services, where our expert liver specialists can provide medical therapy and additional treatment options.
How much does a liver transplant cost?
The costs of liver transplant surgery vary depending on your insurance, but they can be very high.
Your UPMC liver transplant credit analyst and social worker will:
- Give you a packet with information about your insurance benefits and potential out-of-pocket costs for your liver transplant.
- Help you with finding resources to help pay for your liver transplant if you can't cover the costs.
- Patients without insurance will be provided with contact information for patient business services and a transplant credit analyst to discuss estimated costs.
- Work with you to understand your insurance coverage.
Waiting for your new liver
If you're a candidate for liver transplant, we will place you on the United Network for Organ Sharing (UNOS) waiting list. Prior to being placed on the waiting list, your insurance company has to provide approval. You will be notified regarding the outcome by phone and mail.
If it is determined you are not a candidate for transplant at this time, you may be asked to return for additional testing to be cleared medically to be placed on the waiting list.
Your blood type and your Model for End-Stage Liver Disease (MELD) score decide your position on the liver transplant wait list. The MELD score is a series of blood tests that measure how your liver works. The higher your score, the higher you will be on the list.
Your UPMC liver transplant team will continue to manage your liver disease while you wait for an organ with your local medical team.
While on the liver transplant waiting list
While on the liver transplant wait list, you need to live within a four- to six-hour travel radius of UPMC Montefiore so you can get to the hospital when we find a liver donor match.
You will need to get blood tests periodically to recertify your MELD score and be seen in the clinic at least every six months so the team can assess your readiness for transplant.
Most patients continue to see their primary hepatologist for follow-up care during this waiting time. Your doctor will remain in contact with the transplant team at UPMC during this time, in addition to your regularly scheduled visits at UPMC.
If you don't live near Pittsburgh, please find a way to move closer. Family House is an affordable "home away from home" for liver transplant patients and their families. It is not a medical facility.
Learn more about traveling to Pittsburgh for transplant services.
How long will I need to wait for a transplant?
Liver transplant waiting list times are hard to predict and highly variable — from one day to over a year.
Some factors that affect your wait time for a liver transplant include your:
- Blood type.
- Health status.
- Size and weight
Finding a living donor can reduce or eliminate your wait time for a new liver.
Why should I consider a living donor for my liver transplant?
In any given year, the number of people seeking a liver transplant is far higher than the number of available deceased-donor livers. This can result in wait times of over a year.
If you're facing end-stage liver disease, a living-donor transplant may be the best option to improve your quality of life.
A living liver donor must:
- Be between the ages of 18 and 55.
- Be in good health.
The donor does not have to be a family member. They can be a friend, coworker, or even a stranger. People interested in becoming a liver donor are carefully evaluated to make sure they can safely donate.
Benefits of living-donor liver transplant at UPMC include:
- Ability to do the transplant even if the donor is not of a compatible blood type.
- Highly experienced transplant team.
- Improved long-term outcomes.
- Less chance of becoming very sick or dying while waiting for a new liver.
- Less time spent on the transplant waitlist.
- Low risk to the donor.
- Surgery can be scheduled at a time that is convenient for both the recipient and the donor.
Your liver transplant surgery
Your UPMC transplant coordinator will call you when a donor liver becomes available. We will provide you with directions on where to report when you arrive at the hospital.
If you're able to find a living donor for a liver transplant, you have flexibility in scheduling the surgery.
Before coming to the hospital
Before coming to the hospital for your liver transplant:
- Bring all of your medications.
- Do not eat or drink.
- Pack your cell phone and charger.
When you arrive at the hospital
When you arrive at UPMC, you will be admitted to a patient room where you will:
- Have a history and physical done.
- Have basic testing.
- See an anesthesiologist.
- Sign consent forms for the liver transplant surgery.
How long does liver transplant surgery take?
Liver transplant surgery takes six to 12 hours, depending on your care needs.
During your liver transplant surgery
During a liver transplant, your surgeon will:
- Make an incision in your abdomen.
- Cut off the blood vessels to your diseased liver.
- Remove the diseased liver and replace it with the healthy donor liver.
- Reattach the bile ducts and blood vessels.
- Close the incision.
Your coordinator or surgeon will be able to provide more details about your specific surgery.
Advanced techniques for complex liver transplants
UPMC's team of liver transplant experts performs many complex liver transplant operations. We're equipped to handle the risks of surgery and address any complications.
We also offer “bloodless” surgery for patients who meet strict health requirements. Bloodless medicine means we do not use banked blood products during the operation.
Your recovery after liver transplant surgery
Your hospital stay
You will stay in the hospital for about two weeks after your liver transplant.
At first, you'll be in the transplant intensive care unit (ICU) as you recover from the operation. Here, the liver transplant team will closely monitor you and your new liver.
You will start taking antirejection medications right away to help reduce the chance of liver rejection.
When your body detects something new, your immune system begins working to fight what it views as a threat. Antirejection drugs suppress your immune system's natural response to allow your body to accept the new liver.
After your condition is stable, you'll move to a patient room on the transplant floor.
During this time, your liver transplant care team will:
- Help you get up and move around. Being too still right after surgery will increase your risk for blood clots.
- Manage your meals to help you work your way back to eating solid foods.
- Work with you to create a treatment plan for you to follow when you go home.
Going home from the hospital
Before leaving the hospital, your liver transplant care team will review:
- Eating and nutrition guidelines.
- Your medication schedule.
- Tips for becoming more active and things you can and cannot do.
- Your follow-up visit schedule.
Be sure you fully understand your treatment plan before you leave the hospital.
Your care partner's role
You must have a care partner with you 24 hours a day for at least six weeks after you leave the hospital.
Being a care partner is a big responsibility. You may need more than one person to help you for the first few months after your liver transplant.
A liver transplant care partner will:
- Assist with daily activities within the home.
- Arrange your transportation to and from your follow-up appointments.
- Help you record all the information that the transplant team requests.
- Help you stick to your posttransplant treatment plan.
- Keep family and friends informed of your needs and wishes.
- Look for signs of health complications and contact your UPMC transplant coordinator if anything seems wrong.
- Make sure you take medications in the proper doses at the correct times.
- Provide support, encouragement, and entertainment.
- Run errands, fill prescriptions, and do chores around the house.
- Shop for food and prepare meals.
Your follow-up care
After you are discharged from the hospital, you need to stay close to UPMC for at least a few months for follow-up care. Family House offers affordable long-term housing for liver transplant patients and their families. Family House is not a medical facility.
The frequency of your follow-up visits depends on how quickly you recover.
In most cases, you will visit UPMC's posttransplant clinic:
- Once a week for the first month.
- Every two weeks starting in month two.
- Once a month after six months.
- From nine to 12 months, your doctor will determine the frequency.
You must come to these follow-up appointments.
During your follow-up appointments, you will:
- Complete additional testing as needed.
- Consult with a transplant surgeon or transplant hepatologist.
- Have blood work.
- Meet with your transplant coordinator.
This process enables the liver transplant team to diagnose and treat any problems right away to make sure that:
- You are healing as expected after surgery.
- You aren’t developing an infection.
- Your body isn’t rejecting your organ.
- Your new liver is working properly.
- Your body is responding well to the new medicines.
Our team at UPMC will take care of you for at least the first year after transplant, and ideally for life. In some special circumstances, you may be able to find a local transplant center that can take care of you.
Antirejection medications
As soon as you come out of liver transplant surgery, you will begin taking medication to suppress your body's immune system. You will continue to take the antirejection drugs you received in the hospital for the rest of your life. Your doctor will continuously monitor how you respond and make adjustments.
Life after liver transplant surgery
Your liver transplant care team at UPMC will give you a detailed, personalized guide on caring for yourself at home. Make sure you and your care partner fully understand every part of it.
Always look for signs of infection or rejection and call us if you have any questions or concerns.
Your recovery will depend on your health before liver transplant and how dedicated you remain to your care plan.
To make the most of your new liver, it is important to follow your treatment plan and maintain a healthy lifestyle.
Healthy lifestyle tips after liver transplant
Healthy lifestyle tips after liver transplant surgery include:
- Take all medicines on time as prescribed — You will take many of these medicines for the rest of your life. Ask a nurse, pharmacist, or your transplant coordinator if you have any questions about your medicines.
- Stick with your healthy lifestyle changes — Follow the health and lifestyle recommendations the UPMC liver transplant team gave you before your transplant.
- Follow your personalized meal and diet plan — If you have questions, contact your nutritionist.
- Eat healthy and avoid alcohol — To achieve the fullest life with your new liver, you should also limit salty or sugary foods and eat lean proteins.
- Achieve your weight and exercise goals — Try to exercise at least a few days a week as you heal. Stay active to avoid weight gain and reduce your risk of stroke or heart attack.
If you have any questions about caring for yourself at home, call us. We value our responsibility as your transplant team and are here as a resource for the rest of your life.
When to call your doctor about complications
You should let your surgeon know if you have:
- A fever of more than 100.0°F.
- Difficulty breathing.
- Numbness, tingling, pain, swelling, or weakness in your arms or legs.
- Pain, redness, bleeding, drainage, or increased swelling at your surgical site.
- Severe pain that does not respond to medication.
What’s the survival rate after liver transplant?
The survival rates for living-donor liver transplants at UPMC are notable. The one-year survival rate is 87% to 93%, and the five-year survival rate is more than 75%.
Why Choose UPMC for Liver Transplant Surgery?
When you choose UPMC for liver transplant care, you will receive:
- Access to experienced, board-certified specialists — UPMC’s liver surgeons have pioneered minimally invasive (laparoscopic) liver surgery and have performed this technique more than 250 times — making them one of the most experienced teams in the United States.
- Expert care for complex cases — Our program is one of the oldest and largest in the United States. Since the program's inception in 1981, more than 6,000 adults have received liver transplants — including more than 1,000 living-donor liver transplants. This experience allows us to treat patients with complex liver conditions, including those with advanced liver cancer.
- Personalized liver transplant care — From thorough evaluation to world-class treatment, we provide a patient-centered approach to care throughout the entire transplant process. Your dedicated transplant team will guide and support you each step of the way.