What Is a Lung Transplant?
A lung transplant involves removing one or both diseased lungs and replacing them with new, healthy ones, typically from a deceased donor. You may get one or two lungs during your transplant, depending on your condition. For patients with advanced lung disease, a transplant is their only long-term treatment option.
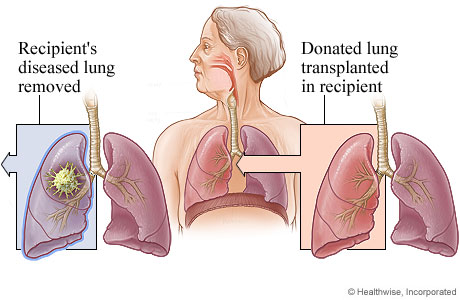
Lung Transplant
For a lung transplant, the recipient's diseased lung is removed and replaced with the donated lung.
© 2016-2025 Healthwise, Incorporated. This information does not replace the advice of a doctor.
Types of lung transplant
There are several types of lung transplant, including:
- Single-lung — One diseased lung is replaced by a donor lung.
- Double-lung — Both diseased lungs are replaced by donor lungs.
- Heart-lung — Both diseased lungs and the heart are replaced with donor organs.
- Living-donor lobar lung transplant (LDLLT) — A portion of the lower lobe of a living donor lung is used to replace the recipient’s diseased lung. Often, two living donors are required for one recipient. The procedure is typically only an option for children or smaller individuals.
Conditions we treat with lung transplant
A lung transplant may be able to help people who have:
Why Would I Need a Lung Transplant?
When you have end-stage lung disease and no longer see results with medical therapy, you may meet the criteria to be a lung transplant candidate at UPMC.
Who’s a candidate for a lung transplant?
At UPMC, we consider each person referred to our lung transplant services — even if you have been turned down at another center.
You may be eligible for a lung transplant if you have a life-threatening lung condition that can’t be treated with medication or other therapies and have a life expectancy of less than three years.
You must also be:
- In good overall health.
- Cancer-free for at least five years.
- Nicotine-free for at least six months.
- Drug-free with no use of marijuana, cocaine, heroin, or other illicit substances.
- Willing to make healthy lifestyle changes after your transplant.
Is there an age limit for a lung transplant?
At UPMC, we consider the risks and benefits for each patient separately. All patients are considered on a case-by-case basis, and age is one of many factors. In general, patients over age 70 must have a limited number of other medical problems to be candidates for a lung transplant.
Who is not eligible for a lung transplant?
You may not be eligible for a lung transplant if you have:
- Active infections.
- A body mass index (BMI) above 35.
- Cancer.
- Current nicotine or substance use.
- Uncontrolled chronic health conditions.
- Severe mental or psychiatric illness that would prevent you from following your pre- or post-transplant treatment plan.
What Are the Risks and Complications of Lung Transplant?
Although many lung transplants occur with little to no problems, there are some risks, including:
- Infection.
- Primary graft dysfunction — Occurs when the lungs don't function right away.
- Rejection of the donor lung(s).
These complications occur in about 10% to 20% of lung transplant surgeries. They result in longer hospital stays, increased recovery time, and, in some cases, death.
UPMC uses innovative surgical methods and medications to help reduce the risk of or quickly respond to these complications.
What Should I Expect from Lung Transplant?
UPMC is one of the most recognized and experienced centers in the world, evaluating many high-risk patients, including those requiring re-transplantation. The earlier you are referred to our program, the better your chances of a good transplant outcome.
The first step in the process is for your doctor to refer you to UPMC. We also accept self-referrals.
Lung transplant patient information review
After our lung transplant team receives your medical records and information listed on the transplant referral checklist:
- A transplant nurse coordinator will collect your medical history, radiology studies, recent blood work, and current physical findings.
- The lung transplant team will review the information to determine if a transplant evaluation is appropriate.
- If a transplant evaluation is appropriate, we will obtain insurance authorization and contact you to schedule the evaluation.
Lung transplant evaluation
The UPMC Lung Transplant Program works closely with the UPMC Comprehensive Lung Center to provide exceptional care and treatment for the entire spectrum of lung diseases. This includes comprehensive evaluations for transplantation.
At UPMC, we evaluate patients with traditional and complex lung conditions, as well as those requiring retransplantation.
Does my care partner need to come to my lung transplant evaluation?
We require all candidates to be accompanied by a primary care partner. The evaluation is physically demanding, and it would be difficult for someone with lung disease to get from one appointment/test or location to the next without assistance or help with their equipment.
It is also essential for the primary care partner to attend the pre-transplant education class, meet with the transplant team members, and learn what to expect as a potential care partner post-transplant. Being a care partner is a big commitment, and the team will not advocate for listing a candidate who does not have strong care partner support.
Your lung transplant evaluation and care team
During your evaluation, you'll have various diagnostic tests and meet with a number of experts from the lung transplant team, including:
- Behavioral health nurses or psychiatrists — Assist you and your family in coping with the stresses associated with chronic disease and the transplant process. They will also assess any current psychiatric/mental health symptoms that are being treated or may need to be treated.
- Credit analysts — Review your insurance coverage and benefits information. They will help you understand your insurance policy and serve as your primary point of contact for any insurance-related changes. They will also explain any parts of the transplant process that insurance does not cover and suggest options to assist with those costs.
- Lung transplant nurse coordinator — Introduce you to the transplant process and review your evaluation schedule. The visit will include a preliminary health screening, a review of your medication, and an overview of the transplant process. Your transplant nurse coordinator is here to answer any questions you may have.
- Lung transplant surgeons — Assess your physical capability and risks for transplant. They will review your lung disease and the medical management of your diagnosis and address all treatment options available to see if a lung transplant is the best option for you.
- Nutritionists — Assess your nutritional status, dietary knowledge, and provide education and recommendations for your diet.
- Pharmacists — Meet with you to get a complete list of all the medicines and supplements you take, both prescription and over-the-counter, and ask you how you take your medicines.
- Social workers — Discuss your support team at home, your prescription insurance coverage, and other social aspects of the transplant process. You will also learn about fundraising options.
- Transplant pulmonologist (lung specialist) — Will examine you, perform a medical history and physical, and focus on the signs and symptoms of your lung disease. They may also review other options for managing your lung disease.
Lung transplant evaluation testing
Testing will include:
- Blood tests — To determine your blood type and check for signs of disease, infection, or other problems.
- Cardiac (heart) tests— To make sure your heart is healthy before surgery.
- Imaging tests — To assess your lung health and look for signs of other health problems.
- Pulmonary function tests — To check how well your lungs are working.
- Six-minute walking test — To see how well your lungs work during exercise.
After your lung transplant evaluation
A multidisciplinary team reviews each patient’s case at a selection meeting and makes decisions regarding approval of lung transplant candidates. We will notify you of our decision shortly after the evaluation.
For patients who are either too sick or are too healthy and not eligible for a lung transplant, our transplant team can refer them to our lung services. There, our expert lung specialists can offer medical therapy and other treatment options for lung disease.
How much does a lung transplant cost?
The cost of a lung transplant can vary from patient to patient, depending on insurance coverage and other factors. If a potential candidate wishes to discuss the estimated cost, they will be provided with contact information for patient business services and a transplant credit analyst.
Lung transplant waiting list
If you're a candidate for a lung transplant, we will place you on the United Network for Organ Sharing (UNOS) waiting list. Before being placed on the waiting list, your insurance company has to provide approval. You will be notified regarding the outcome by phone and mail.
If it is determined you are not a candidate for transplant at this time, you may be asked to return for additional testing to be cleared medically to be placed on the waiting list.
Your UPMC lung transplant team will continue to manage your lung disease while you wait for an organ with your local medical team.
While on the lung transplant waiting list
While on the lung transplant wait list, you need to live within a four-hour travel radius of UPMC so you can get to the hospital when we find a lung donor match.
You will need to get tests periodically and be seen in the clinic at least every six months so the team can assess your readiness for transplant.
Most patients continue to see their primary pulmonologist for follow-up care during this waiting time. Your doctor will remain in contact with the transplant team at UPMC during this time, in addition to your regularly scheduled visits at UPMC.
If you don't live near Pittsburgh, UPMC offers affordable long-term housing options. Family House is an affordable "home away from home" for lung transplant patients and their families. It is not a medical facility.
Learn more about traveling to Pittsburgh for transplant services.
How long will I need to wait for a lung transplant?
Waiting times are hard to predict and can vary greatly, from one day to over a year. The average is a few months, but this depends on your condition.
Your lung transplant surgery
Your UPMC transplant coordinator will call you when a donor lung or lungs become available.
Before coming to the hospital
Before coming to UPMC for your lung transplant:
- Do not eat or drink anything.
- Take an antimicrobial shower.
- Pack your cell phone and charger.
- Bring all your medications.
The surgeon will evaluate the donor lung(s) to make sure they are the right size and type and that the antibody panel is a match.
When you arrive at the hospital
When you arrive at UPMC, we will admit you to a patient room where you will:
- Have a history and physical done.
- Have basic testing.
- See an anesthesiologist.
- Sign consent forms for the lung transplant surgery.
We will prep you for your lung transplant and give you general anesthesia.
How long does a lung transplant take?
How long your lung transplant surgery takes depends on the complexity of your case.
- For a single-lung transplant, surgery will take six to eight hours.
- For a double-lung transplant, surgery will take eight to 12+ hours.
During your lung transplant
During a lung transplant procedure, your surgeon will perform the following steps:
- Make an incision in your chest.
- Cut off the airways and blood vessels to your diseased lung(s).
- Remove the diseased lung(s) and transplant the healthy donor lung(s).
- Reattach the airways and blood vessels.
- Close the incision.
Your coordinator or surgeon will be able to provide more details about your specific surgery.
During the procedure — most often with a double-lung transplant — we may connect you to a heart-lung machine. This machine supports your heart and lungs during surgery. It oxygenates your blood outside your body and pumps it back into your body.
Advanced techniques for complex lung transplants
UPMC's team of lung transplant experts performs many complex lung transplant operations. We're equipped to handle the risks associated with surgery and address any potential complications.
We use special techniques and surgical tools for transplanting lungs in people with small chests.
We also offer “bloodless” surgery for patients who meet strict health requirements. Bloodless medicine means we do not use banked blood products during the operation.
Your recovery after a lung transplant
Your hospital stay
After a lung transplant, we will take you to the transplant intensive care unit (ICU), where you will stay for several days. Here, you will remain on a ventilator until you can breathe on your own. This may take a few hours to a few days.
We will give you pain medicine and anti-rejection drugs right away.
When your body detects your new lung(s), your immune system begins working to fight what it views as a threat. Antirejection drugs suppress your immune system's natural response to allow your body to accept the new lung(s).
When you're stronger, you will move to a patient room within the transplant unit. You can expect to stay in the hospital for three to four weeks.
The lung transplant team will monitor your progress to make sure your body isn't rejecting the lungs and that you aren't developing an infection or other problems.
You'll begin rehabilitation, which includes physical therapy, breathing exercises, and speech therapy.
As you recover, your care team will help you get up and moving to prevent blood clots and keep your smaller airways in your new lungs from collapsing.
You may be kept at NPO status (nothing by mouth) for days to months post-transplant to ensure that your swallowing function is working correctly and to prevent aspiration of food or drink into your new lung(s).
Going home from the hospital
Before leaving the hospital, your lung transplant care team will review your:
- Diet and exercise guidelines.
- Follow-up visit schedule.
- Medication schedule.
Be sure you and your care partner fully understand your at-home care plan before you leave the hospital.
You'll also need to care for the incision site to prevent infection. Follow the directions your transplant nurse gave you before you left the hospital.
Staying close to UPMC
The first few months after lung transplant surgery are when you have the highest risk for infection or rejection. That's why you will need to remain within one hour of UPMC for at least two to three months after discharge or as directed by your transplant team.
You must also have a care partner with you at all times during these first few months.
Family House offers a "home away from home" near the hospital, providing a comfortable stay until you're ready to return home. It is not a medical facility.
Your care partner's role
An organ recipient needs a lot of help after transplant surgery. Being a care partner is a big responsibility. You may need more than one person to help you for the first few months after your lung transplant.
A lung transplant care partner will:
- Assist with daily household activities.
- Drive you to and from your follow-up appointments.
- Help you record all the information that the lung transplant team requests.
- Help you stick to your post-lung-transplant treatment plan.
- Keep family and friends informed of your needs and wishes.
- Look for signs of unusual behavior and contact your UPMC lung transplant coordinator if anything seems wrong.
- Make sure you take medications in the right doses at the right times.
- Provide support, encouragement, and entertainment.
- Run errands, fill prescriptions, and complete household chores.
- Shop for food and prepare meals.
Your follow-up appointments
At first, you will have frequent follow-up visits so the lung transplant team can make sure you're healing properly.
After that, you will return to UPMC's post-transplant clinic at least every two months for a two-day visit for the first year. This timeline may vary based on your testing results at any visit.
Our team at UPMC will take care of you for at least the first two years following transplantation, and ideally for life. In certain special circumstances, you may find a local transplant center that can assist you with your care.
Follow-up testing
Lung biopsy is the only way for your doctor to determine whether your body is accepting or rejecting your new lung(s). That's why it's so important that you come to all your follow-up appointments.
During these visits, you will have:
- Blood work.
- Bronchoscopy with biopsy.
- Chest x-rays.
- Clinic visits.
- Pulmonary function testing (PFT) to make sure your lung function continues to improve.
Antirejection medications
You will continue taking the antirejection drugs you received at the hospital for the rest of your life. Your doctor will regularly monitor your response and adjust the treatment as needed.
The antirejection drugs make you more susceptible to developing infections.
After lung transplant surgery, limit your exposure to people with illnesses or places where people are likely to be spreading germs.
Call us if you have any signs of infection, which include:
- Chills.
- Fever over 100.4°.
- Swelling, redness, or fluid draining from the incision site.
Life after lung transplant
Most people who receive a lung transplant at UPMC have good results and can gradually return to their normal routines within three to six months.
To make the most of your new lung(s), it's important to follow your treatment plan and maintain a healthy lifestyle.
Be sure to:
- Take all medications as prescribed — If you have any questions, call our office.
- Stick with your personalized nutrition plan — Follow the recommendations your nutritionist created for you, based on your medications.
- Avoid all nicotine products — This includes cigarettes, cigars, smokeless tobacco, e-cigarettes, nicotine patches, gum, or any other form of pharmaceutical nicotine. You should also avoid all forms of vaping, even if products claim to be nicotine-free.
- Exercise regularly — Begin with your breathing exercises and short walks, as you're able. Your care team may suggest that you complete a pulmonary rehab program.
Remember that the UPMC lung transplant team is here for you for the rest of your life.
When to call your doctor about complications
You should let your surgeon know if you have:
- A fever of more than 100.4°F.
- Difficulty breathing.
- Numbness, tingling, pain, swelling, or weakness in your arms or legs.
- Pain, redness, bleeding, drainage, or increased swelling at your surgical site.
- Severe pain that does not respond to medication.
What’s the survival rate after lung transplant?
The median survival rate after a lung transplant is approximately seven years and varies from a few days to more than 25 years.
Lung transplant resources for patients and families
Download these resources to learn more about the lung transplantation process, our medical team, and the resources available to help patients and care partners.