What Is Thoracic Endovascular Repair for Aortic Aneurysms (TEVAR)?
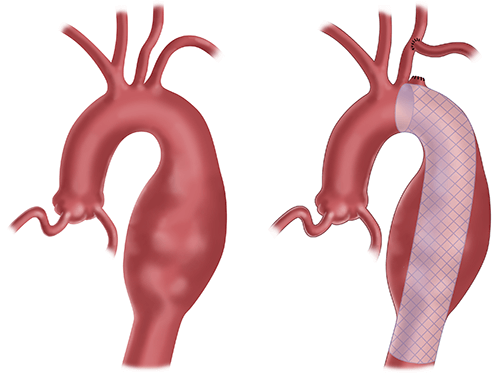
An aortic aneurysm is a bulge in the aorta, the artery that carries blood from the heart to the rest of your body. An aortic dissection is a tear in the inner layer of the aorta. Both these conditions are dangerous and need to be treated.
TEVAR is a minimally invasive surgery to fix an aortic aneurysm or an aortic dissection in your chest without open surgery.
Instead of making a large incision, surgeons insert a catheter into an artery in your groin. They then place a stent into the dilated aorta to seal off the aneurysm and prevent further growth or rupture.
Conditions we treat with TEVAR
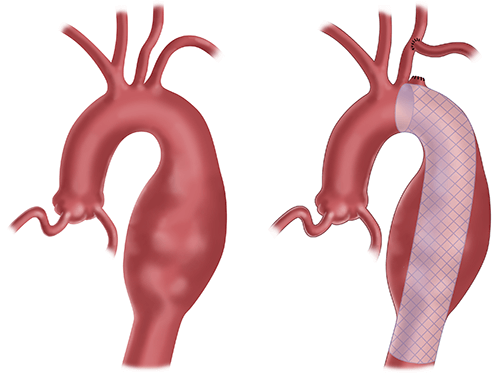
A descending thoracic aortic aneurysm is a bulging, weakened area in the wall of the aorta, in the section that runs downward through the chest.
Why Would I Need TEVAR?
Depending on the size of your aneurysm, doctors may only need to watch it periodically. But if it grows quickly or to a large size, surgeons may need to treat it with open surgery or TEVAR.
TEVAR may be the right choice for you if:
- The aneurysm is 50 percent larger than the rest of your artery.
- The aneurysm is more than five centimeters (about two inches).
- You have a connective tissue disorder, such as Marfan syndrome, Loey-Dietz syndrome, or Ehlers-Danlos syndrome.
- Your aneurysm is growing quickly.
Who’s a candidate for TEVAR?
You may be a candidate for TEVAR if you have a thoracic aortic aneurysm or aortic dissection in your chest that is large or growing.
What is the difference between TEVAR and endovascular aortic aneurysm repair (EVAR)?
TEVAR is used to repair thoracic aortic aneurysms. These occur in the upper part of the aorta. EVAR is performed to treat abdominal aortic aneurysms. These occur in the lower part of the body.
Alternatives to TEVAR
- Open chest surgery (sternotomy) approach for aortic aneurysm repair.
What Are the Risks and Complications of TEVAR?
Like all surgeries, TEVAR does involve some risk. Complications of TEVAR may include:
- Infection.
- Bleeding.
- Blood vessel injury.
- Aortic dissection.
- Aneurysm rupture.
- Stent failure or migration during deployment.
- Kidney damage from dye used during surgery to guide stent placement.
- Paralysis of the lower body.
If your surgeon believes you are at high risk for postoperative paraplegia, you may also need a lumbar drain placed in your spinal column. The drain will help protect your spinal cord during and after TEVAR.
Neurophysiology specialists are present during all TEVAR procedures. This specialized team checks the motor responses of all extremities during the procedure. If they notice any signs of neurological problems, surgeons can immediately intervene.
What Should I Expect From TEVAR?
Your surgeon will plan your aortic aneurysm or dissection treatment based on your:
- Precise diagnosis.
- Anatomy.
- Other health problems.
Treatment may involve either:
- Watchful waiting — Your doctor will monitor your condition with CT scans and control your blood pressure with drugs.
- Surgery — Your doctor will recommend TEVAR or an open chest aortic aneurysm repair.
Before: How to prepare for TEVAR
If you and your surgeon agree that endovascular repair is the best way to treat your aortic aneurysm, you'll need pre-surgical testing. Tests may include:
- Blood work and urine studies — Your doctor may order blood work and urine studies to ensure you are healthy enough for surgery and check for signs of illness or infection.
- Chest x-ray — A chest x-ray is a diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs on film. An x-ray can show enlargement in any area of the heart.
- CT scan — CT scans create images of your heart.
- Echocardiogram (ECHO) — This noninvasive ultrasound test uses sound waves to evaluate your heart's chambers and valves. The ECHO sound waves create an image on a monitor as an ultrasound transducer is passed over your heart.
- Electrocardiogram (ECG or EKG) — This test records the electrical activity of your heart, shows abnormal rhythms (arrhythmias or dysrhythmias), and can sometimes detect heart muscle damage.
- Lung function studies — Lung function studies show your doctor how well your lungs work to ensure you are healthy enough for surgery.
- Doppler ultrasound — This test uses sound waves to create pictures of your arteries and find blockages.
- Cardiac (heart) catheterization — This test is a diagnostic procedure that allows your doctor to see blockages, blood flow, and other problems within your arteries.
Your doctor will explain the TEVAR procedure to you and answer your questions. To prepare for TEVAR you should:
- Tell your doctor if you are sensitive or allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
- Tell your doctor about all medications (prescription and over-the-counter) and herbal or other supplements you are taking.
- Tell your doctor if you have a history of bleeding disorders or if you are taking any blood-thinning medications, aspirin, or other medications that affect blood clotting. You may need to stop some of the medications prior to the procedure.
- Fast for a certain time before the procedure. Your doctor will tell you how long to fast (usually overnight).
- Have any tests that your doctor recommends. For example, your doctor may request a blood test before the procedure to determine how long it takes your blood to clot.
On the day of your TEVAR surgery, bring your photo ID and health insurance card(s). Leave valuables such as cash and jewelry at home.
After your TEVAR valve procedure, you will stay in the hospital for about a week. Your doctor will let you know how many nights you may expect to stay.
You should bring toiletries, a robe, slippers, a cell phone and charger, medications, and a change of clothes. You should also arrange for someone to drive you home from the hospital after you are discharged.
How long does TEVAR take?
TEVAR typically takes about two hours.
During your TEVAR
On the day of your surgery, before going into the OR:
- A nurse will place an IV in your arm and may draw blood.
- An anesthesiologist and a member of the surgical team will examine you. They'll answer last-minute questions and help you sign consent forms.
- If our team determines that you need a lumbar drain, a member of the care team will place a small catheter in your back to drain fluid from around your spinal cord. This helps improve blood flow to the spinal cord after surgeons place the stent and decreases the chances of leg paralysis.
The anesthesia team will put you to sleep using general anesthesia. They will then place a breathing tube down your throat and place you on a ventilator. This machine will breathe for you during surgery.
A nurse will insert a catheter in your bladder.
During TEVAR, your surgeon will:
- Make a small cut in your groin and place a sheath in your femoral artery.
- Advance a wire through the sheath into the aorta and thread a stent over the wire.
- Use ultrasound, radiograph, and contrast dye to locate exactly where the stents should go.
- Place one or more stents to seal off the aneurysm and prevent further growth or rupture.
Recovery after TEVAR
After your surgeon finishes your operation:
- The OR staff will remove your breathing tube and take you to the ICU.
- For select patients who have a lumbar drain placed, you will remain in the ICU until the drain is removed.
You will stay in the hospital for about a week after your procedure. You will have cardiac rehabilitation and physical therapy during your hospital stay to help you regain your strength.
After your discharge
After you are discharged from the hospital:
- You'll need to take it easy at home for 4 to 6 weeks (about 1 and a half months).
- A home nurse will visit you 2 to 3 times per week for 2 to 4 weeks. These visits will include vital signs, exams, medication monitoring, and blood draws.
- You may also need home occupational or physical therapy.
Common symptoms during recovery
During your recovery, you may have:
- Groin pain where your surgeon made the incision.
- Shortness of breath.
- Fatigue or lack of energy.
- Swelling in the arms, hands, legs, or feet.
- Trouble sleeping.
- Short-term mood changes, including anxiety or depression.
Post-op care instructions
It's vital to follow your surgeon's instructions during recovery. That means:
- No driving until after your 4-week follow-up visit with your surgeon. It's fine to ride in a car in the meantime.
- Don't lift anything heavier than 10 pounds.
- Lift your legs above your heart whenever you sit.
- Take brief walks each day to regain your strength.
- Blow into your incentive spirometer at least 10 times per hour. Using this device fills your lungs with air and helps prevent post-op issues like pneumonia.
Follow-up tests and visits
You will have your follow-up visit 4 to 6 weeks (about 1 and a half months) after leaving the hospital. You may need to have some tests done before that visit, such as:
- CT angiogram.
- Echocardiogram (ECHO).
- Electrocardiogram (ECG or EKG).
If your test results are normal, you can resume driving after this visit. You can also return to work and most other normal activities.
You can expect to have your next appointment in 6-12 months. You must also schedule visits with your heart doctor and primary care provider.
When to call your doctor about TEVAR complications
You should call your doctor if you are experiencing any unusual symptoms, including:
- Pain, redness, bleeding, drainage, or increased swelling at the insertion site.
- Chest pain.
- Difficulty breathing.
- Fainting.
- Severe pain, coldness, numbness, or discoloration in the limb where the catheter was inserted.
- A fever of more than 100.0°F.
If any of these symptoms are severe or if you experience loss of consciousness, you should dial 911 immediately.
What’s the prognosis after TEVAR?
After TEVAR, many patients can live full, active lives with routine follow-up care. You may need to avoid strenuous activity and take medication to reduce the risk of another aortic aneurysm.
What’s the success rate of TEVAR?
The TEVAR is a highly successful procedure for reducing the risk of aortic rupture. However, you may need to have routine follow-up care.
What is the survival rate of TEVAR?
The 30-day survival rate after a TEVAR procedure is 93-94 percent.
Why Choose UPMC for TEVAR?
The surgeons at UPMC are at the forefront of advanced and life-saving surgical techniques for aortic aneurysm repair. We provide personalized care tailored to your condition, using minimally invasive techniques whenever possible.
By UPMC Editorial Staff. Last reviewed on 2024-10-01.